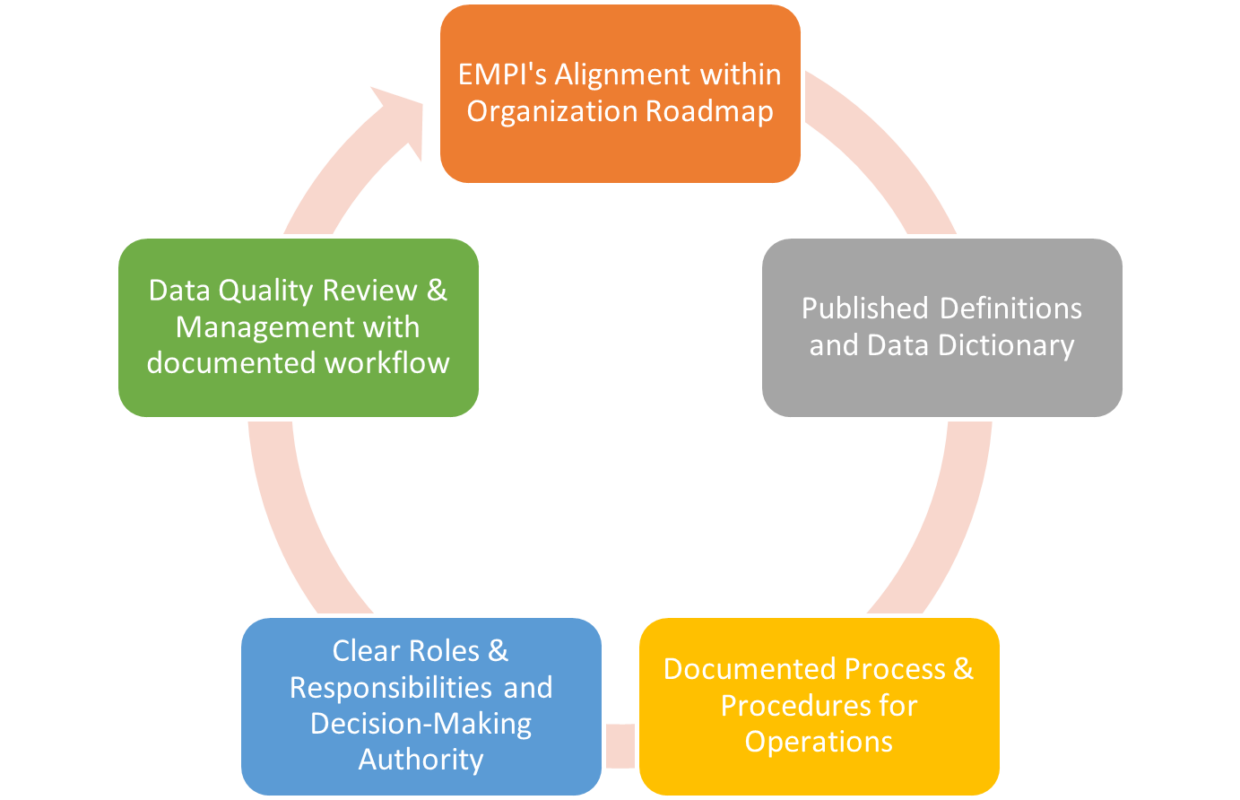
By Minakshi Tikoo You probably hear the buzz about data governance. It almost sounds too bourgeois, and many treat the construct as a big-to-do. Simply put, it is a process that facilitates creation of agreed…
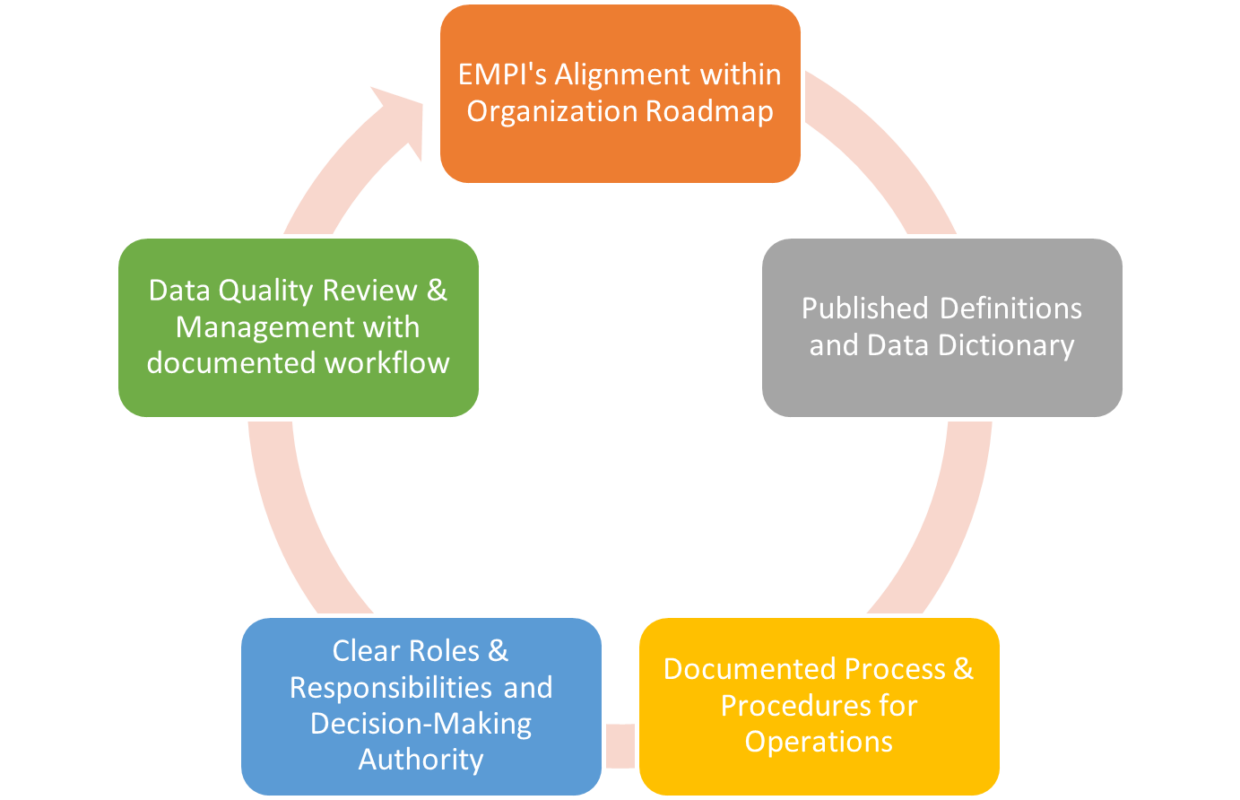
By Minakshi Tikoo You probably hear the buzz about data governance. It almost sounds too bourgeois, and many treat the construct as a big-to-do. Simply put, it is a process that facilitates creation of agreed…
Yesterday, I went to get my booster shot at NYC’s City Point vaccine hub in Brooklyn. This time I remembered to take my two vaccine cards, as I did not want to collect a third…
Telemedicine first began as a form of healthcare delivery in the late 1960s. While it was initially introduced by the National Aeronautics and Space Administration (NASA) and the Nebraska Psychology Institute, perhaps it would have…
Our nation’s COVID response is a failure of the U.S. public health system. Last week, the pandemic reached a grim milestone: 700,000 coronavirus-related deaths have now been reported in the U.S. I happened to be…
Identity theft is so common in our daily lives that it’s not a matter of “if” it will happen, but “when”. In fact, the number of identity theft cases more than doubled in 2020 from…
Healthcare’s heavy reliance on clipboards, signatures, and plastic ID cards can cause significant frustrations for patients and providers including incorrect patient matching, medical errors, repeated services, and poor communication. Today’s consumers demand convenience. The rise…
Last month, the Office of the National Coordinator for Health Information Technology (ONC) released its first Project US@ Technical Specification draft for public comment. The initiative aims to improve patient matching, while supporting interoperability, privacy…
How can we as an industry improve data sharing and eliminate paper-based forms that consumers routinely fill out when they seek care? What level of pain or loss of capital is required to force institutions…
Keeping physician credentials and affiliations up to date has been a long standing source of angst for payers and providers alike. Research estimates that 2 to 2.5 percent of provider data changes each month, and…